Abortion and Breast Cancer: Are They Connected?
Share this Article:
Is Abortion and Breast Cancer Connected?
The connection between abortion and breast cancer is a hot topic surrounded by much debate. The question is concerning since we have conflicting messages that “abortion is safe or healthy” and that abortion is “not safe or unhealthy.” The abortion industry suggests any such connection between breast cancer and abortion is a myth. Forgive us for not taking their word for it since they have a financial stake in abortion on demand. Fortunately research on the question is ongoing, and it is demonstrating
that abortion and breast cancer are connected.
In 2011 Life News reported 53 of 66 studies done in 54 years show breast cancer and abortion are connected[1]. More research has been introduced since 2011 supporting this connection. The strength of that connection is being studied using the scientific method. In the meantime we can review what we know, and use it to inform our choices. Pregnancy Care Clinic believes women and men deserve access to the information about this concern. We also believe people are smart enough to understand and use this information knowing stronger support is in progress.
Research and Bias
There are numerous studies that have been conducted around the world to answer the question, “Is abortion and breast cancer connected?” These studies have been conducted by the US government, the abortion industry, the pro-life community, universities and private research groups. They have been published in peer reviewed scientific and medical journals. The majority of these studies demonstrate breast cancer and abortion have a relationship among those who have had one or more induced abortions. However, some studies show no relationship between abortion and breast cancer. The discrepancy between these studies comes down to bias in the research. Bias is where outside influences, affects the results of the data. There are many kinds of bias in research. Bias can be intentional or it can be something overlooked. Bias can also be a factor that was not possible to remove. Examining the “method” section of research articles is where most bias can be found. Of significant concern in studies on abortion and breast cancer is “recall bias.” This is where the subject of a study does not recall the details of past events reliably. This unreliability could be purposeful, like not wanting to talk about something uncomfortable. The subject could also forget.
The second common bias found in these studies is sample bias. This occurs when a sample size is too small, or leaves out a part of the population that might change the results. For example, in 1997 a Danish study[2] that claims there is no connection between breast cancer and abortion was found to have sample bias. The sample bias involved only sampling electronic records where paper charts going further back contained records where abortion had been performed on subjects who had breast cancer later in life.
Research on both sides have been discredited due to sample bias and recall bias. Bias can never be eliminated. Good research projects are designed to eliminate as much bias a possible in order to produce clear data. Additionally, good researchers will say where they recognize that bias still exists in their research. Nearly all research includes a call for more research to get a better understanding, and to demonstrate repeatability.
Learning from the past
The scientific process has at its core a thirst for knowledge specific to questions we have about our world. Research into the connection between abortion and breast cancer is informed by research done in the past, and peer review of that research. New research addressing bias is designed where bias was discovered in previous research. Learning that research is biased does not entirely discredit it. The whole body of research on a topic of science is important to take into account.
In the last decade numerous studies have been done where recall bias is addressed. In these examples, controlled populations are studied that are reliably seeking care from facilities. All the health records are crosschecked. Recall bias is removed since the subject is never asked a question by the researcher. Instead the researcher looks at the medical records of women who have had an abortion then after a period of time check the record for any sign of breast cancer. Or the opposite, a subject is found to have breast cancer, then medical records are reviewed to search for an abortion. The reliability of the medical records, and size of the population determines the strength of the data. Recent studies on small closed populations of this kind have been conducted in Turkey[3], India[4] and China[5]. More time and more studies on breast cancer and abortion are needed to know what exactly the connection between the two are, and how strong it is.
Cause and Effect
Without getting into a long philosophy lesson , establishing a cause and effect relationship in research statistics is very difficult. Generally the best conclusion statistical analysis can provide is if two or more things are correlated or not. Correlation or association does not mean there is a cause and effect relationship in the data. Marketing and poor journalism have done much to confuse the difference between correlation and cause and effect. We are often presented half truths to sell products or are misled to make specific decisions that fit an agenda. When we hear, “studies show…”, “research proves…”, or ” X is caused by Y… ” we should raise our eyebrow and ask questions about what exactly is demonstrated in the research.
Correlation: a mutual relationship or connection between two or more things
Pregnancy Care Clinic does not assert that abortion causes breast cancer. We do however feel strongly that people considering abortion need to know the majority of studies done on this subject indicate abortion and breast cancer are correlated or related[1]. The trouble is (as stated above), correlation does not prove causation. So what does that do for our question about the safety of abortion? Is the correlation between abortion and breast cancer enough or is it proof that it is a myth? Fortunately there are reasoning tools we can use to determine how important the correlation is:
- Is the explanation for the correlation reasonable? Since breast cancer and abortion are correlated, we can review the reason they are connected to determine if we should pay attention to it. Our medical director explains the reason here.
- Given enough time, a cause and effect relationship can be proven. This will require more research studies for repeatability. Additionally other potential causes for breast cancer need to be ruled out.
- Consider the strength of the correlation. If a study shows a high percentage of women who had an abortion also get breast cancer, that is a strong correlation. If repeated studies also show a similar high percentage, the strength of a cause and effect relationship is building.
- We can weigh the information and determine how much it matters to us if it is true. In other words, if the correlations were to be proven as a cause relationship, would that change your behavior?
- We can ask what are the risks if we change our behavior due to correlated data, but the correlation is not proven to be cause and effect.
Should abortion be avoided because of correlations to breast cancer?
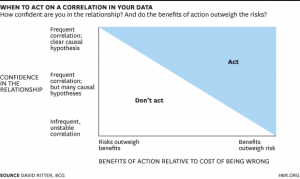
The truth is, we make a lot of decisions about life using data that is correlated. When we combine all the above reasoning tools at our disposal, we can determine if a correlation means we need to act or not act. David Ritter who is a contributor to Harvard Business Review has an excellent article on business decisions based on correlation. The same principles apply to all decision making including if abortion should be avoided due to a potential risk of breast cancer.
What do we Know for Sure?
- Carrying a baby to term, but more specifically carrying your first baby to term, provides protection against cancer cells forming in breast tissue.[6]
- Breast feeding your baby also provides protection against cancer cells forming in breast tissue.[7] The longer into the first year the better.[4]
- Breast tissue grows and develops rapidly in the first trimester. Learn more about breast development and growth from the Medela website (leading producer of breast pumps) here.
- Near the end of pregnancy (at 32 weeks) the breasts are mature enough to produce milk, and are resistant to developing breast cancer.[8]
- Induced abortion artificially stops breast development resulting is a loss of protection against breast cancer.
- First Trimester miscarriages are spontaneous and do not increase a woman’s risk of developing breast cancer.[9]
If you would like to discuss these things further, make an appointment to discuss your concerns about abortion with our professional staff.
References:
1. Lafranchi A. (2011). Abortion-Breast Cancer: 53 of 66 Studies in 54 years show link. Life News , October 18
2. Melbye M., et. al. (1997). Induced Abortion and the Risk of Breast Cancer. New England Journal of Medicine , 336:81-85
3. Ozmen V. et. al. (2009). Breast cancer risk factors in Turkish women: a University based nested case control study. World Journal of Surgical Oncology, 7:39
4.
Jabeen S., et. al. (2013). Breast Cancer and Some Epidemiological Factors: A Hospital Based Study. Journal of Dhaka Medical College
, 22(1) 61-66
And
Bhadoria A., et. al. (2014). Reproductive Factors and Breast Cancer; A case-control study in tertiary care hospital of North India. Indian Journal of Cancer
(4) 316-321
5. Huang Y., et. al. (2014). A Meta-analysis of the Association Between Induced Abortion and Breast Cancer Risk Among Chinese Females. Cancer Causes and Control , 25(2) 227-236
6.
National Cancer Institute. (2016). Reproductive History and Breast Cancer Risk. National Cancer Institute
, November 9
And
Troisi R., et. al. (2013). A Linked-registry study of Gestational Factors and Subsequent Breast Cancer Risk in the Mother. Cancer Epidemiol., 22(5), 835-847
And
Costarelli V., Yiannakouris N. (2010). Breast Cancer Risk in Women: The Protective Role of Pregnancy. Nursing Standard
, 24(18), 35-40
7. Antsey E. H., et. al. (2017). Breastfeeding and Breast Cancer Risk Reduction: Implications for Black Mothers. Am J. Prev Med. 53(3), S40-S46
8.
Hsieh C., et. al. (1999). Delivery of premature newborns and maternal breast-cancer risk. Lancet
, 353:1239
And
Russo J., et. al. (2000). Develomental, molecular and cellular basis of human breast cancer. Journal of National Cancer Institute Monographs.
27, 17-37
9. Kitchen, A. J. et. al. (2005). Is There A Link Between Breast Cancer and Abortion: a review of the literature. Int J Fertil Womens Med, 50(6), 267-271